How Long Does Hip Dysplasia Last in Babies
Introduction [edit | edit source]
DDH (developmental dysplasia of the hip ) is a disorder that is due to abnormal development of acetabulum with or without hip dislocation. Early diagnosis and direction will prevent long term complications eg persistent dislocation,limp and early hip osteoarthritis.[1]
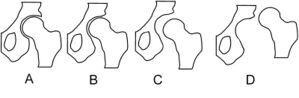
Epitome 1: Schematic depiction of hip joint structures' positions in hip dysplasia A - Normal, B - Dysplasia, C - Subluxation, D - Luxation
- DDH alters hip biomechanics, overloading the articular cartilage and leading to early osteoarthritis. DDH is the chief cause of total hip replacement in immature people (about 21% to 29%)[2].
- Presentation varies from modest hip instability to frank dislocation. The exact etiology is all the same elusive. Multifactorial in nature, a combination of genetic, ecology, and mechanical factors plays a part.[one]
Clinically Relevant Anatomy [edit | edit source]
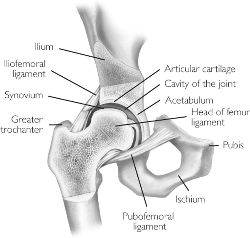
The Hip joint is a classical ball-and-socket articulation. Information technology meets the four characteristics of a synovial or diarthrodial articulation: it has a joint crenel, joint surfaces are covered with articular cartilage, it has a synovial membrane producing synovial fluid, and information technology is surrounded by a ligamentous sheathing.[three]
- Acetabulum and femoral head development are intimately related. Development of the acetabular cavity is determined by the presence of a concentrically reduced femoral head. When the femoral caput is not in contact with the acetabulum, the latter does not develop adequately and it is flat-shaped[2].
- A deep concentric position of the femoral head in the acetabulum is necessary for a normal development of the hip. When the bone structures of the hip are fully grown, we can speak of a brawl and socket joint between the rounded head of the femur and the cup-like acetabulum of the femur.[iv]
- The proximal femur is completely cartilaginous at birth[2].
Pathology [edit | edit source]

The germination of the hip joint is highly dependent on the dynamic relationship between femur and acetabulum. Whatever interference with proper contact between these two in utero or infancy leads to DDH.
Maligned contact for a prolonged menstruation leads to chronic changes like hypertrophy of capsule, ligament teres, the formation of thickened acetabular border (neolimbus), which further prevents the contact, and prevents the relocation of the femoral caput[1]. The very cellular hyaline cartilage allows the femoral head to glide out of the acetabulum generating the palpable clunk known as the Ortolani sign.[5]
Image 3: Hip displasia adult
Epidemiology [edit | edit source]

The reported incidence of developmental dysplasia of the hip varies between 1.v and xx per thou births, with the majority (sixty-eighty%) of abnormal hips resolving spontaneously within ii-8 weeks (so-called young hip).
The incidence varies from 0.06 in Africans to 76.one per 1000 in Native Americans due to the combination of genetics and swaddling.[5]
Etiology [edit | edit source]
The post-obit are the take a chance factors for DDH:
- Female gender (M: F ratio ~1:8) The increased incidence is probably due to ligamentous laxity from maternal hormones.[1]
- Firstborn baby. The incidence of DDH is 10 times more in new borns with breech malposition
- Family unit history. eg Certain ethnic populations (Native Americans and Sami people). Some studies suggest it is linked with the hormone relaxine and /or it has something to do with chromosone xiii
- Breech presentation. The legs of the foetus are pressed inside the uterus leading to hip dislocation if the ligaments are lax. The caput femoris tends to be pushed out of the acetabulum.
- Whatsoever physical limitation (eg oligohydramnios, twins) in utero tin can contribute to DDH. It also increases the risk of other abnormalities like Metatarsus adducts, congenital muscular torticollis, and congenital knee dislocation.
- Spina bifida[5]
- Swaddling in the adducted and extended position. Explains the increased incidence in specific populations including American Indians, Japanese and Turkish infants[1].
- Structural abnormalities eg shallow acetabulum, a flat or irregular caput femoris, a femoral or acetabular anteversion, and a decreased caput first or perpendicular distance from the heart of the femoral head to the axis of the femoral shaft.[6] [7] [8]
Characteristics/ Clinical presentation [edit | edit source]
Clinical features vary for mild hip instability, limited abduction in the infant, less mobility or flexibility on ane side, limping or toe walking, and osteoarthritis in the adult.[one]
Developmental dysplasia of the hip is usually suspected in the early on neonatal period due to the widespread adoption of clinical examination (including the Ortolani test, Barlow manoeuvres, and Galeazzi sign).[five]
Diagnostic procedures [edit | edit source]
All newborns are to exist screened by physical test. This test includes an Ortolani or Barlow test.
If these tests are negative but the provocation test is positive, an ultrasonography is recommended. Ultrasound is the modality of pick prior to the ossification of the proximal femoral epiphysis. Once in that location is a pregnant ossification then an ten-ray examination is required.
Other signs of hip dysplasia are asymmetric gluteus folds and an apparent limb-length inequality.
[9]
Treatment/Management [edit | edit source]
The goal is to provide an optimal environment for the growth of the femoral head and acetabulum. So a high index of suspicion and routine surveillance is needed to detect DDH and prevent complications.
All treatment efforts are based on obtaining a concentrically positioned femoral head into the acetabulum and then the latter is stimulated to abound usually. Acetabular potential of correction diminishes dramatically later on 3 to four years of age; therefore, early on interventions are paramount to obtain the best results with less surgical aggression[2]. Various treatment modalities like abduction splinting, closed reduction, open reduction are available.
Double diapering is almost likely harmless, but efficacy is close to nothing.[1]
The treatment depends on the age of the patient and the degree of dysplasia.
- Modest hip instability (Barlow positive, Ortalani negative) spontaneously recovers in ninety% of cases in the offset two weeks of life.
- Continued surveillance by the primary care provider during infancy improves detection and early on referral.
- Pavlik harness corrects 95% of DDH if applied earlier vi months.
- Remainder dysplasia occurs even after appropriate handling, and then annual follow up is required until skeletal maturity.
- Without early treatment, the child may develop limp, leg length discrepancy, express hip abduction, and in fact, DDH is the most common crusade of early osteoarthritis in women under age forty.[1]
The college the age at presentation, the worse the outcomes after intervention for DDH. By the historic period of eight years, information technology is idea that possible complications of treatment may pb to a poor outcome, no better than if DDH is left untreated[2]
This is a video (three minutes) re DHD from the mothers view of her neonatal girl.
[ten]
Physiotherapy for DHD in Babies [edit | edit source]
Even though DHD is mutual and ordinarily very well managed, it can be difficult and overwhelming for new parents to deal with the dos and don'ts forth with the other struggles of parenthood. With physiotherapy we tin help the parents experience empowered and enable them to assistance their babies along the process of healing.
Although it is non standard practise for a paediatrician to refer to a physiotherapist just a visit to a physiotherapist subsequently the diagnosis gives parents a better insight and can assist with managing the condition at home specifically during the splint free time at home.
Research has shown that appropriate massage, stretching and strengthening tin help with the recovery of the hip while the child is in the brace. All these treatments tin can be performed by the parents at domicile once perfected by a visit to the physiotherapist every month.
A baby can exercise and strengthen the hip muscles past using their developmental milestones to their reward. A physiotherapist should do a thorough assessment of the baby, go through the scans, follow the recommendations by the paediatrician and make a plan that suits the baby according to their age[eleven].
eg a baby with hip dysplasia needs to exist kept in a certain position to give their hip a mechanical reward. So if information technology is a baby who is 6 months former, the physiotherapist takes reward of their current milestones and trains the hip muscles on a number of surfaces keeping the hip position in mind and challenge the hip muscles. This besides avoids the chances of delayed milestones that can happen in babies with serial and prolonged periods of casting.

Image 4: Baby wearing a Pavlik harness
When the child is younger than six calendar month the use of a special brace called a Pavlik harness is used.[12] The brace holds the hips of the babe in the right position. Over time the articulation begins normal formation. Nearly ninety% of the newborns treated with the Pavlik harness will recover fully. Also a Frejka Pillow is used but is not indicated in all forms of hip dysplasia.
When the child is older then half-dozen months the Pavlik harness may not exist successful. In that case a surgeon will identify the hip in the proper position under anesthesia. Once in this position the child will be placed in a spica cast. The spica bandage is like to the Pavlik harness but allows less motility.

Image v: Traction A form of treatment for Hip dysplasia
A handling that isn't often used is traction. Traction exists of the application of a force to stretch certain parts of the body in a certain direction. This volition soften the tissue around the caput femoris and will allow the head femoris to motility back in the acetabulum. Traction consists of pulleys, strings, weights, and a metal frame attached over or on the bed. Traction is almost often used for approximately 10 to 14 days. The application of ice on the painful regions helps to numb pain and reduces the inflammation.[13]
Physiotherapy for older child/adult DHD [edit | edit source]

Therapy is of import to correct poor posture, muscle weakness, poor articulation awareness, and associated tendon inflammation. Therapy can improve all these factors including the force of hip extensors and external rotators, gait re-education, and improving body awareness. Strong muscles will act like stupor absorbers and provide greater support for the hip.
If osteoarthritis of the hip is present see this connection for Physiotherapy
- Practise: Regular, low- or non-impact exercise such equally swimming, aquatic therapy or cycling train strength and range of motion.
- Weight loss: For those overweight can significantly reduce the stress on the hip and reduce pain.
- Hippotherapy: A specialized therapy treatment strategy that uses a horse's movement to influence the patient/client in a diverse number of ways.[xiv] During hippotherapy, functional riding skills are not taught; the customer sits on the horseback and physically accommodates to the three-dimensional movements of the horse'due south walk. Hippotherapy is shown to motivate the child to engage in therapy, maintain the child's willingness to participate and provide a playful surround while facilitating pain complimentary motion.[15]
References [edit | edit source]
- ↑ 1.0 one.1 1.2 1.three 1.four 1.5 1.vi 1.seven Nandhagopal T, De Cicco FL. Developmental Dysplasia Of The Hip. StatPearls [Internet]. 2020 Oct 10. Available: https://world wide web.ncbi.nlm.nih.gov/books/NBK563157/(accessed 11.10.2021)
- ↑ 2.0 2.1 2.2 2.3 2.iv Vaquero-Picado A, González-Morán K, Garay EG, Moraleda L. Developmental dysplasia of the hip: update of direction. EFORT open up reviews. 2019 Sep;iv(9):548-56. Bachelor: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6771078/ (accessed 12.10.2021)
- ↑ Byrd J. Gross anatomy. In: Byrd J, editor. Operative Hip Arthroscopy. 2nd ed. New York: Springer Science + Business organisation Media, Inc; 2004.
- ↑ American University of Pediatrics, Committee on Quality Improvement, Subcommittee on Developmental Dysplasia of the Hip, Clinical Practice Guideline : Early detection of developmental Dysplasia of the hip, Official Journal of the American Academy of Pediatrics Vol 105 No 4 April 2000, downloaded from pediatrics.applications.org at Swets Blackwell 30680247 on November 23, 2011. Level of testify: one A
- ↑ v.0 5.1 5.2 5.three Radiopedia Developmental dysplasia of the hip Available: https://radiopaedia.org/manufactures/developmental-dysplasia-of-the-hip (accessed 11.10.2021)
- ↑ John Crawford Adams, David L. Hamblem, Outline of Orthopaedics, Churcill Livingstone, 1995, twelfth edition, p. 292 – 301.
- ↑ John Crawford Adams, David L. Hamblem, Outline of Orthopaedics, Churcill Livingstone, 2001, thirteenth edition, p. 305 – 312.
- ↑ J.Maheshwari. Essential Orthopaedics. 6th edition. Jaypee Brothers Medical Publishers,2019
- ↑ Dr. Anisuddin Bhatti. Ortolani'southward Click & Barlow's Maneuver. Bachelor from: http://world wide web.youtube.com/watch?v=mv_kLqZSGdo [last accessed 04/05/thirteen]
- ↑ Childrens Hospital. Angela and hip dysplasia - Boston Children'due south Hospital. Bachelor from: http://www.youtube.com/watch?v=bShtxYFdERQ [final accessed 04/05/13]
- ↑ Inner Strength Physiotherapy for hip dysplasia in babies: a style to empower parents to assist their little humans. Bachelor: https://www.innerstrengthbayside.com.au/physiotherapy-for-hip-dysplasia-in-babies-a-mode-to-empower-parents-to-help-their-little-humans/(accessed 12.11.2021)
- ↑ Guille JT, Pizzutillo PD, MacEwen GD. Developmental dysplasia of the hip from birth to half dozen months. JAAOS-Periodical of the American University of Orthopaedic Surgeons. 2000 Jul i;viii(iv):232-42.
- ↑ Enseki KR, Martin RL, Draovitch P, Kelly BT, Philippon MJ, Schenker ML. The hip joint: arthroscopic procedures and postoperative rehabilitation. Journal of Orthopaedic & Sports Physical Therapy. 2006 Jul;36(7):516-25.
- ↑ Debuse D, Chandler C, Gibb C. An exploration of German and British physiotherapists' views on the furnishings of hippotherapy and their measurement. Physiotherapy theory and practice. 2005 Jan 1;21(four):219-42.
- ↑ Roy Aldridge PT, Farley Schweighart SP, Megan Easley SP. The effects of hippotherapy on motor performance and function in an individual with bilateral developmental dysplasia of the Hip (DDH). J Phys Ther. 2011; ii:54-63
Source: https://www.physio-pedia.com/Hip_Dysplasia
0 Response to "How Long Does Hip Dysplasia Last in Babies"
Post a Comment